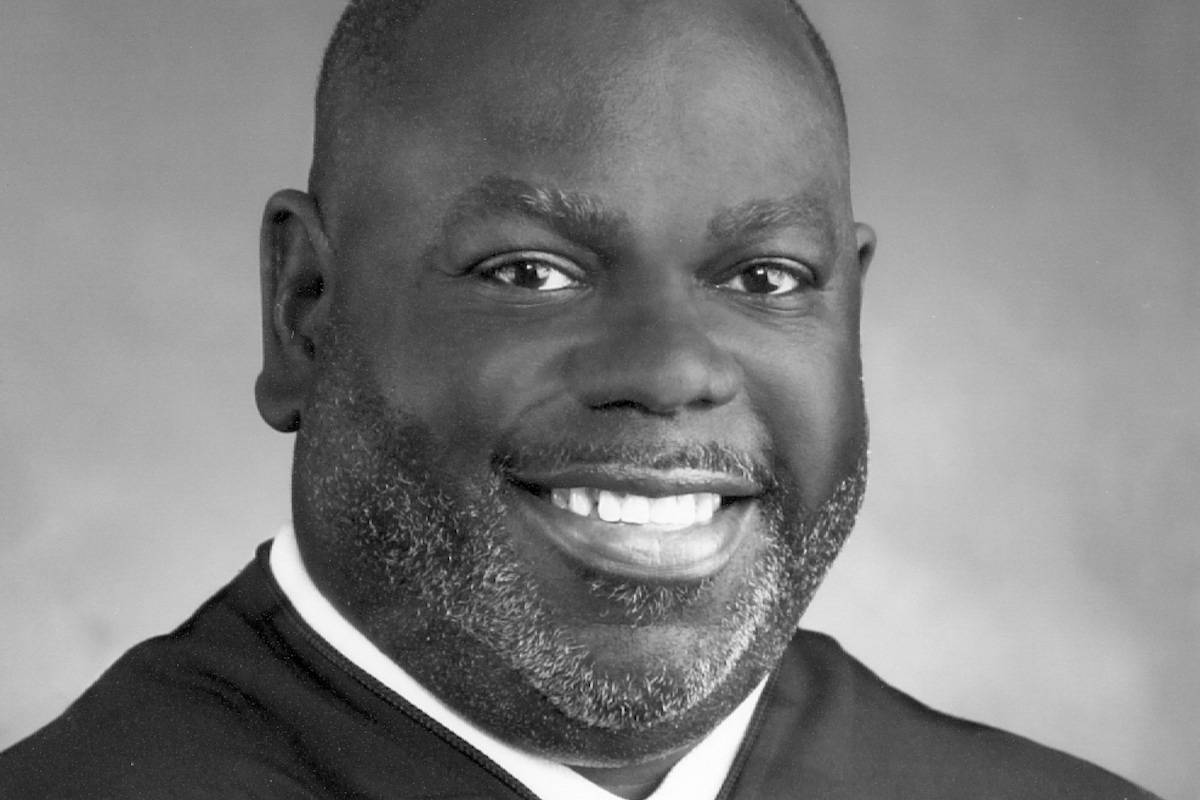
On April 4, 2022, Judge Carlton Reeves held a status conference to review Dr. Michael Hogan’s first monitoring report in the ongoing federal lawsuit against Mississippi’s mental health system. Dr. Hogan monitors the State’s compliance with court-ordered requirements to help adults with mental illness live and work in their communities.
We appreciate that Judge Reeves explained at the beginning of the hearing: “The public is invited to attend this hearing, because in the Court’s view, this is a matter of public concern.” Judge Reeves is right. This case is very much a matter of public concern. We urge public input into this case and the entire mental health system, especially from people receiving services and their families.
Dr. Hogan then reviewed his monitoring process and ended with this summary: “If I were to try to summarize it, the grade for our review so far as well as for the State’s compliance with the order is mostly incomplete. We have seen some signs of early progress.”
He mentioned the impact of the pandemic on the mental health system. “A particularly troubling aspect of this was that people who are waiting for a state hospital bed in some instances had to wait in jail until a bed became available, and this –these challenges are exacerbated by two troubling trends that we’ve found,” he said.
The troubling trends Dr. Hogan discussed are:
- “… a number of state hospital beds are taken up by people who have been committed to that hospital but do not have a serious mental illness. They might have conditions like dementia or a developmental disability or substance abuse problem without having a serious mental illness, and these are people who need care but for whom the state hospital is not the right place, and their being there obviously backs up the system a little bit.”
- “A surprising number of state hospital admissions we’ve found are people who were treated in a private hospital and then transferred to the state hospital. [That’s] perhaps because their insurance ran out [or] perhaps because it’s thought the state hospital has more resources available for discharge, although that’s not necessarily true.”
“We reviewed records at three of the state hospitals during this period and in six of the community mental health centers, and we could see that DMH efforts to improve so-called discharge planning—that is, connecting people back to their community, getting them ready to move back—these efforts have yielded some promise,” he said.
“But we also see that this progress is incomplete,” he said, acknowledging “stressors in the system that ultimately may affect compliance.” He said the pandemic was a significant factor that caused staff shortages.
“Going forward, the monitoring team will build on this initial report,” he said. “As I’d said, in the next few months, a lot of data will begin to flow and be publicly posted and available, and we’ll look at that.”
Patrick Holkins, attorney for the United States Department of Justice, responded with these thoughts:
- “We just want to acknowledge, Your Honor, that the monitor has and the State has taken meaningful steps to implementing the requirements of the Court’s remedial order. Executive director Wendy Bailey and her team have demonstrated their commitment to moving this process forward.”
- “However, even based on the monitor’s reporting available at this time, it is clear that the State has more work to do.”
- “While the United States is encouraged by the State’s implementation of a systemwide discharge planning protocol that incorporates the measures required under the Court’s order, the monitor’s review suggests that adherence with those measures is inconsistent across the state hospitals and CMHS regions surveyed.”
- “The United States shares the monitor’s serious concern about the continued use of county jails to hold civilly committed individuals pending admission to in-crisis state organizations or the state hospital.”
Judge Reeves then asked about forensic beds in the Mississippi state hospital system for people with criminal charges who have mental health challenges. Dr. Hogan explained that is a separate issue beyond this case, and the people in his report waiting in jail for treatment do not have charges.
“The problem that we’ve found is people who are not charged with a crime, simply need care, a bed is not available; and by what I understand is a long-standing practice, they are detained in jail,” Dr. Hogan said. “There’s not much doubt, in my view, that this was exacerbated as a result of beds that were essentially reduced by or in response to COVID.”
After this discussion, Judge Reeves invited Jim Shelson, attorney for the State to respond. Mr. Shelson said:
- “To be clear, to the extent people are waiting in jail, it’s not because there’s a bed available and they’re being denied a bed. I’m not saying Mr. Holkins suggested that, but to the extent he did, we disagree with that. As Dr. Hogan said, they’re there because a bed is not available. It’s not just the state hospital beds. It’s also that there’s no CSU bed available.”
- “Second thing he addressed are people committed to a state hospital who do not have serious mental illness, or SMI. That is a problem. It unfortunately is happening more than certainly the State would like it. But, Your Honor, to be clear, and I mean no disrespect to any court when I say this, that’s — when that happens, it’s a chancellor committing an error of law. It’s not noncompliance by the State with your order.”
- “Last thing is — that Dr. Hogan mentioned that’s troubling is the same-level-of-care issue. That, again, is an unfortunate issue, but it’s not an issue of noncompliance on the State’s part. There are a number of private hospitals who will commit a person to their facility and then after a short period of time will seek to have that person committed to a state hospital. And, again, there’s a number of reasons for that, but if the chancellor commits them, then they’re committed and the state hospital has to do what it has to do.”
Mr. Shelson’s remarks point to a reform issue that we have repeatedly raised: We have no overarching entity to coordinate the different parts of Mississippi’s mental health system. Thus, when conflicts arise—such as between the chancery courts and the public mental health system, or between private and state psychiatric hospitals or even between community mental health centers and the state system—there are no agreed-upon processes and procedures to address them based on the best interest of people needing the services and overseen by an accountable entity.
The conference ended with a discussion of the State’s appeal of Judge Reeves’s ruling (United States’ response) and clarification that both parties agree with parts of the process Dr. Hogan uses to monitor. Dr. Hogan’s next report is due in September and will likely focus on crisis services.